How Ebola in Africa Can Affect You in Central New York
The runaway Ebola outbreak raised new ethical issues. Medical experts say it won’t be the last time, as similar but different epidemics are likely to sprout in America. ProPublica reporter Marshall Allen talked about it with Jeanine Thomas, who serves on a World Health Organization’s ethics committee.

Jeanine Thomas is a well-known patient advocate and active member of ProPublica’s Patient Harm Facebook Community. Last month, she contributed in another forum: the World Health Organization.
The WHO selected Thomas to serve on the ethics committee that recommended making experimental drugs available to Ebola patients in West Africa. Thomas was sole patient representative on the international panel, which decided that offering experimental drugs is ethical if patients give fully informed consent and data is gathered to track the effectiveness of the medications used.
Thomas has a unique perspective. She nearly died from a bacterial infection acquired in the hospital during a routine surgery in 2000. Since then, she has committed her life to speaking out on behalf of patients as founder and president of the MRSA Survivors Network.
Here she discusses why the Ebola decision has relevance for the U.S. health care system, too.
Photo: thinkstock.com
Do you think patients should have access to experimental drugs in situations other than the Ebola outbreak?
I think that should always be an option on the table. There is no drug for the pathogen CRE (carbapenem-resistant Enterobacteriaceae), which can be caught by patients in health care settings, and like Ebola, it’s got a high mortality rate. If there’s a drug out there that could possibly save somebody’s life, and there’s informed consent from the patient or the family member, there should be an option to use it. It’s compassionate care. On the downside, it could cause harm, and that’s why it could only be done in dire situations, and on a limited case-by-case basis.
How is the recommendation made by the World Health Organization ethics committee about Ebola in West Africa relevant to the rest of us?
This will be an issue we face in the future. With CRE, for example, there’s no antibiotic for it, and there will be breakouts. There will also be outbreaks of other superbugs that can’t be treated by known methods because of all the antimicrobial resistance that’s occurred because of the overuse of antibiotics. Who knows what’s going to burst out next? We’re going to need some protocols in place in the future. This is the world we live in now. It’s proven that these pathogens are going to evolve, and there will be no drugs for them.
Photo: thinkstock.com
Why is it important to have a patient advocate on this type of panel?
Patients have a unique perspective that health care industry experts or academics might not have. They know personally what it is to experience a bacterial or viral infection and what happens to the person and how it impacts the family. I’ve personally experienced septic shock, multiple-organ failure and a temperature of 105 degrees. I know how bad these infections can be, and if you survive, it is a very long road to recovery and you are never the same. The pain is unbearable and goes on for months, sometimes years, with lasting effects to your organs and immune system.
The industry and academic experts are more clinical. They’re looking at data, statistics and some have a little detachment. There has to be a voice there that’s a champion for the patient.
Ebola isn’t a threat here, but how worried should we be about these drug-resistant infections in our medical facilities?
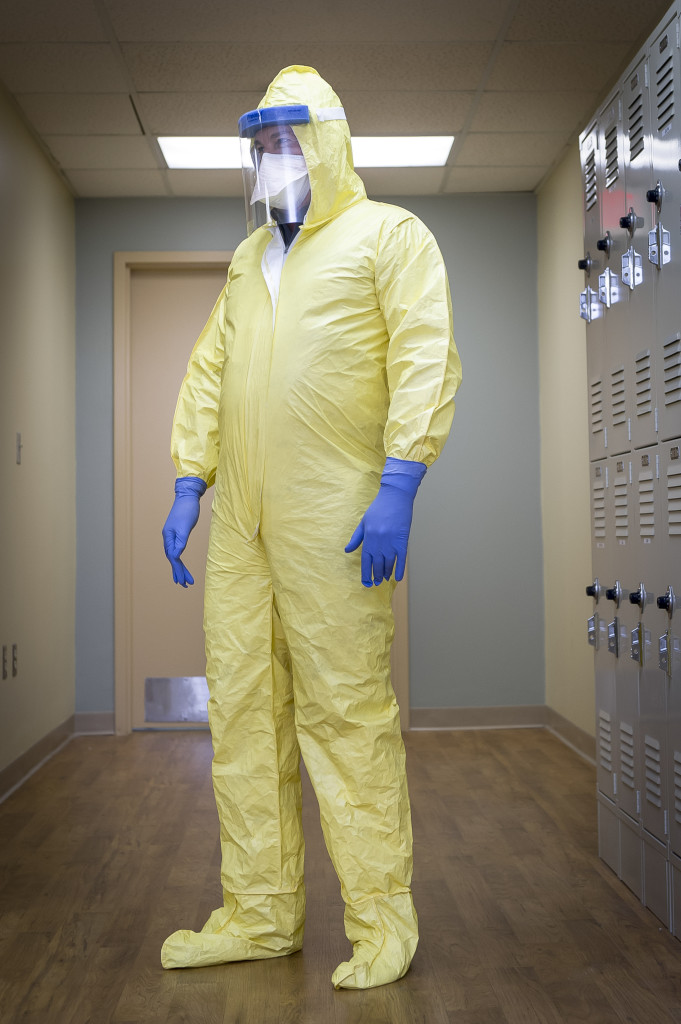
The public should not feel secure in what government health officials say about their ability to control outbreaks here. For decades, we have not controlled MRSA (Methicillin-resistant Staphylococcus aureus) and staph infections in U.S. health care facilities, and now also Clostridium difficile. We are at epidemic levels of MRSA and C. diff infections in many health care facilities.
What steps are the medical community and regulators taking to protect the public from drug-resistant health care-acquired infections?
The Centers for Disease Control and Prevention only gives recommendations, and they’re lax. The CDC has acted for years like hand washing could control health care-acquired infections, and we know that’s not true. The CDC standards are way below those of northern European countries, such as the Netherlands and the Scandinavian countries. In those countries, they screen patients before they enter the hospital and after they’re transferred from one department to another in a facility, and before they’re discharged, to be sure the patient hasn’t been colonized by a bacteria that could be transmitted to another patient or health care facility. They examine clinical cultures to track where the transmissions are happening. They call the method “search and destroy.”
This approach has been proven to work in our country, too. The Veterans Affairs Department hospitals have been screening for MRSA since 2007. They do universal screening, and they have studies that show the method dramatically reduces MRSA infection rates. If the VA is doing it, and it’s a federal agency, why isn’t the CDC strongly recommending this? There is proof! But this screening approach, called active detection and isolation, is still a second-tier recommendation by the CDC. Other places in the world, it’s a first-level recommendation. It should be mandatory here.
Update: According to the CDC, the effectiveness of the type of screening promoted by Thomas is an area of ongoing scientific controversy, said Dr. John Jernigan, director of the agency’s Office of Health Associated Infections Prevention Research and Evaluation. Other independent agencies, including the Agency for Healthcare Research and Quality, have reviewed the research on the subject and agree with the CDC’s recommendations, he said.
ProPublica is an independent, non-profit newsroom that produces investigative journalism in the public interest.



